
影响因子2020
5.788
备受期待的2020年期刊影响因子已经发布,我们很高兴地看到药理学期刊 Pharmacopsychiatry 的影响因子提高到了5.788。非常感谢所有作者、审稿人和编辑的支持和最宝贵的贡献。
以下三篇是被引用次数最多的论文,它们对影响因子的提高有着重要贡献,欢迎免费阅读。
Consensus Guidelines for Therapeutic Drug Monitoring in Neuropsychopharmacology
C. Hiemke et al.
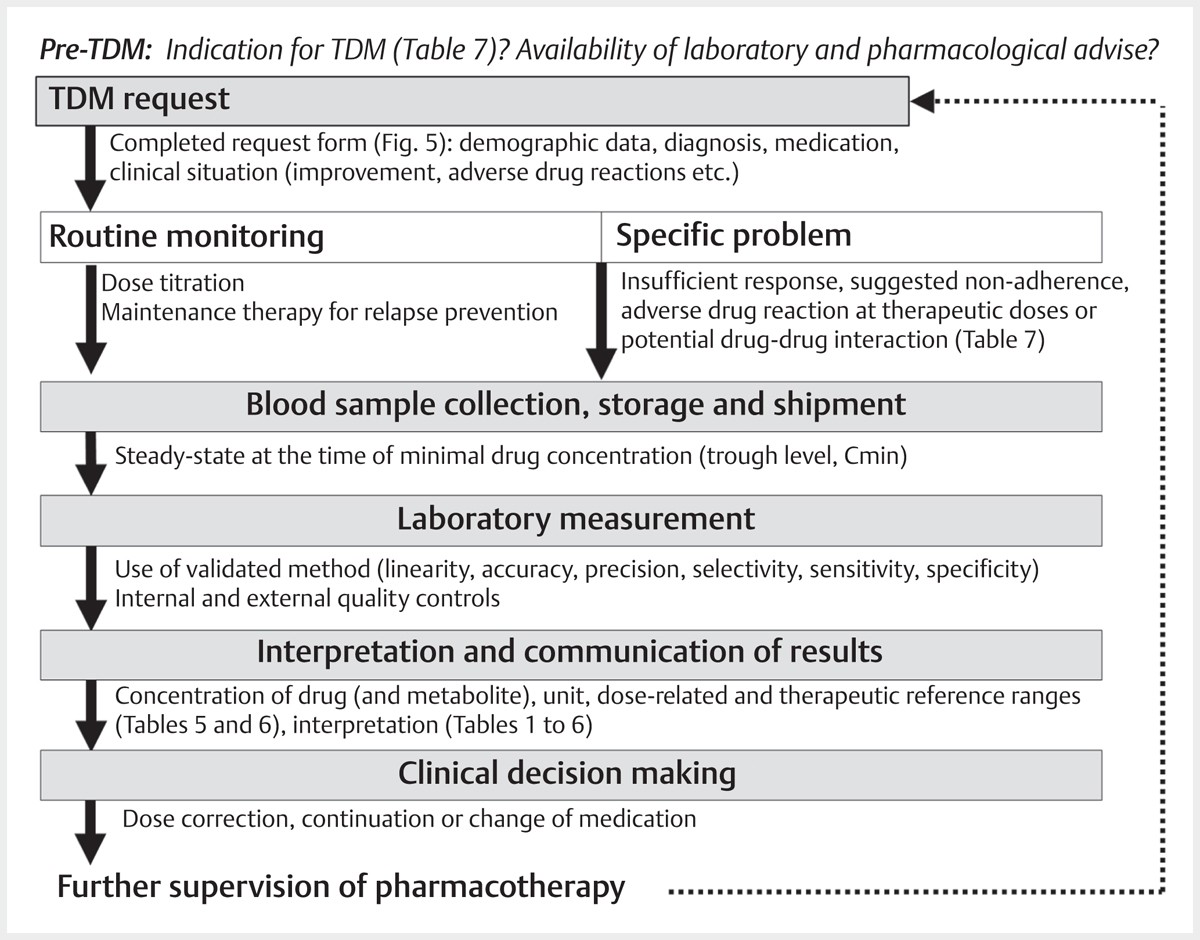
Therapeutic drug monitoring (TDM) is the quantification and interpretation of drug concentrations in blood to optimize pharmacotherapy. It considers the interindividual variability of pharmacokinetics and thus enables personalized pharmacotherapy. In psychiatry and neurology, patient populations that may particularly benefit from TDM are children and adolescents, pregnant women, elderly patients, individuals with intellectual disabilities, patients with substance abuse disorders, forensic psychiatric patients or patients with known or suspected pharmacokinetic abnormalities. Non-response at therapeutic doses, uncertain drug adherence, suboptimal tolerability, or pharmacokinetic drug-drug interactions are typical indications for TDM. However, the potential benefits of TDM to optimize pharmacotherapy can only be obtained if the method is adequately integrated in the clinical treatment process. To supply treating physicians and laboratories with valid information on TDM, the TDM task force of the Arbeitsgemeinschaft für Neuropsychopharmakologie und Pharmakopsychiatrie (AGNP) issued their first guidelines for TDM in psychiatry in 2004. After an update in 2011, it was time for the next update. Following the new guidelines holds the potential to improve neuropsychopharmacotherapy, accelerate the recovery of many patients, and reduce health care costs.
Antisuicidal Effects in Mood Disorders: Are They Unique to Lithium?
Tondo L, Baldessarini RJ.
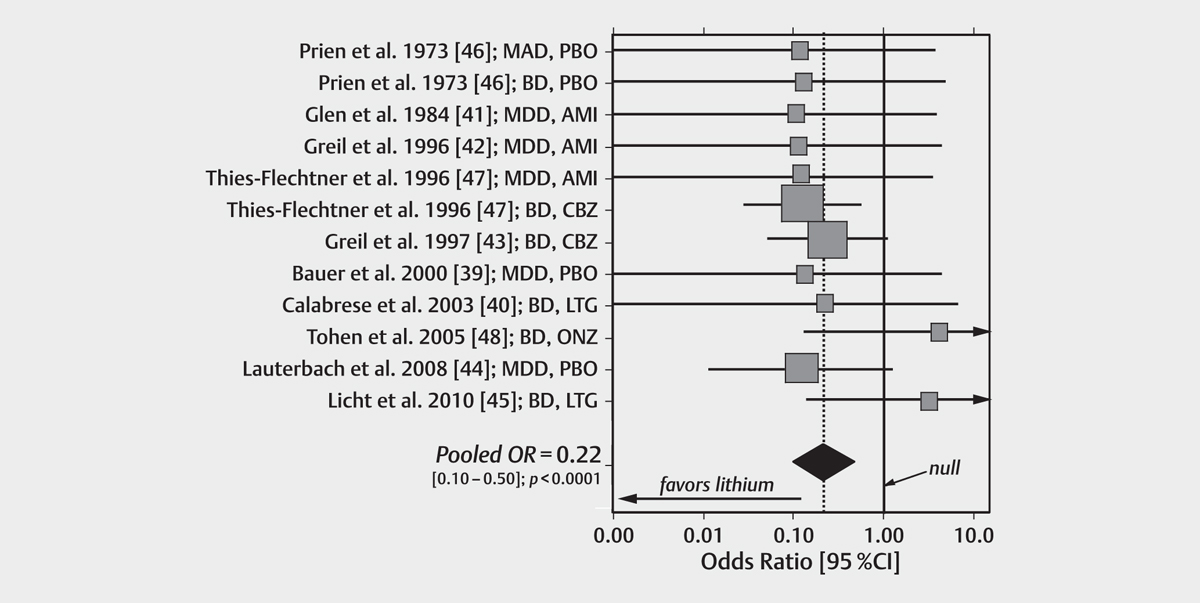
Introduction: Suicidal behavior is strongly associated with depression in major depressive (MDD) and bipolar (BD) disorders, especially with associated behavioral activation, dysphoria, or agitation. A rare intervention with evidence of suicide risk-reducing as well as mood-stabilizing effects in mood disorder patients is lithium.
Methods: We reviewed available research evidence on associations of long-term treatment with lithium with risk of suicidal behavior. We meta-analyzed 12 randomized trials in 10 reports (with at least 1 suicide in either treatment arm) including both BD and MDD subjects, with particular attention to comparisons of lithium with placebo or other pharmacological treatments. We also summarized ecological studies on lithium concentration in local drinking water and reported suicide rates.
Results: We found substantial reduction of risks of suicide and attempts with long-term lithium treatment, particularly in depressive phases of BD and in MDD. Risk of suicidal behavior was higher in mixed (agitated-dysphoric) states than in manic or hypomanic periods. Risk of suicide fatality, specifically, was lower with lithium than with placebo and probably with mood-altering anticonvulsants or antidepressants.
Discussion: Long-term treatment with lithium has growing evidence of suicide- and attempt-sparing effects, probably greater than with anticonvulsants or antidepressants; antipsychotics remain to be tested adequately. However, the ethical and scientifically adequate design and conduct of trials of treatments aimed at suicide prevention remain challenging and underdeveloped.
Efficacy and Effectiveness of Lithium in the Long-Term Treatment of Bipolar Disorders
Severus E et al.
For more than 40 years, lithium has been the gold standard in the long-term treatment of bipolar disorders. In the course of the last 15 years, other drugs have been approved in this indication and are widely used in clinical practice at the expense of lithium. New research from the last few years, however, indicates that lithium is still the first-line treatment in this indication. Against this background and lithium’s proven acute antimanic efficacy, we should perhaps be using lithium more regularly (in combination with an atypical antipsychotic, if necessary) right from the start for the acute treatment of a manic episode and, once remission has been achieved and euthymia maintained during continuation treatment, to regularly taper off the atypical antipsychotic, if possible, and continue with lithium as monotherapy for prophylactic treatment. This might lead to lithium being used more consistently with the scientific evidence in the long-term treatment of bipolar disorders. It remains uncertain, however, to predict who will respond to and tolerate lithium prophylactically, and more research is needed to deliver the best possible individualized care to our patients.
阅读本刊更多论文,请点击这里。
