Thieme旗下心脏病学领域的期刊是研究人员、专家和从业人员公认的首选资源。欢迎免费访问本期的精选论文。
International Journal of Angiology
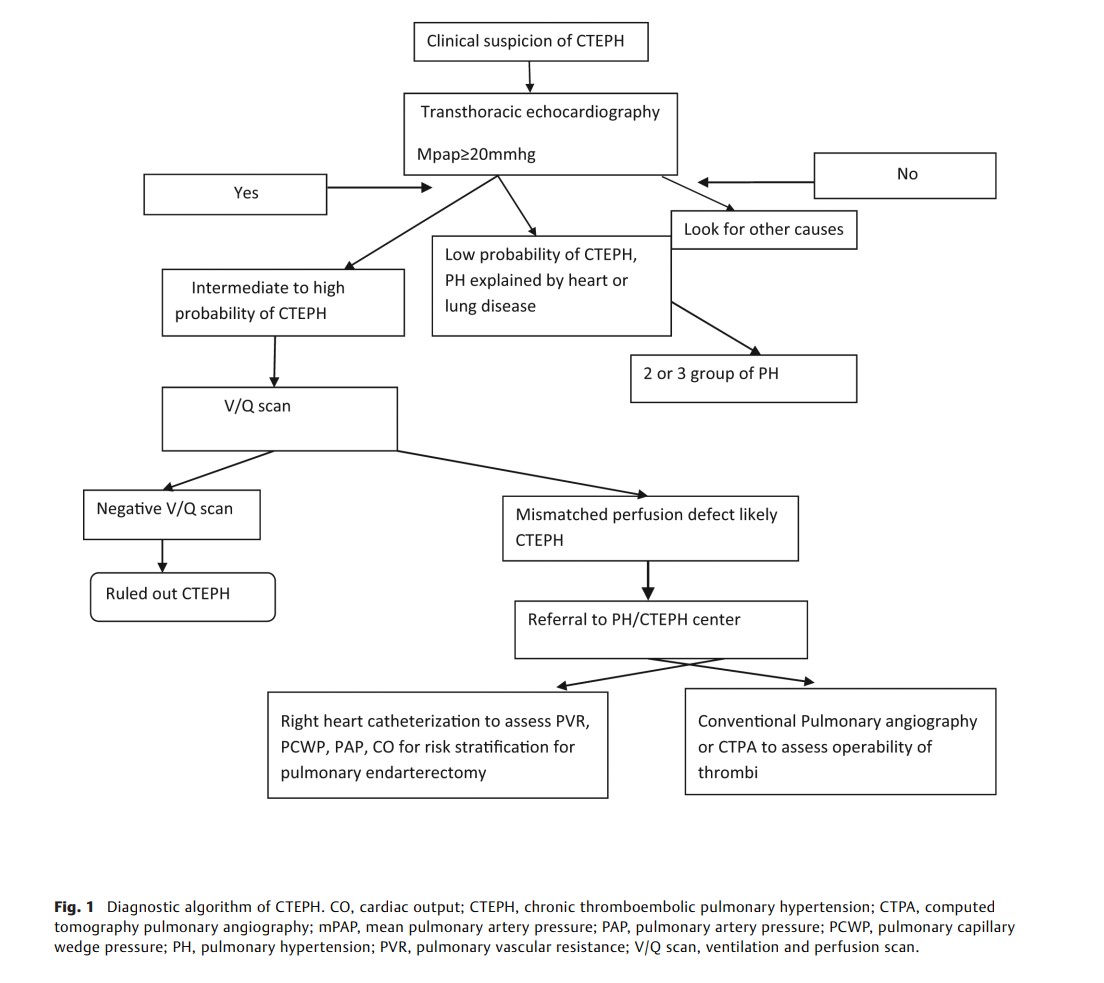
Review of Advances on Management of Chronic Thromboembolic Pulmonary Hypertension
Tyagi et al.
Chronic thromboembolic pulmonary hypertension is rare, underdiagnosed form of pulmonary hypertension. It is caused by intravascular obstruction of pulmonary arteries due to fibrotic transformation of thromboembolic material and microvasculopathy. It is important to diagnose this variant as potentially curative treatment in the form of pulmonary endarterectomy is available. Last two decades have seen rapid advances in targeted medical management and refinement in balloon pulmonary angioplasty technique, which have provided a viable therapeutic option for patients who deemed to be inoperable.
The Thoracic and Cardiovascular Surgeon
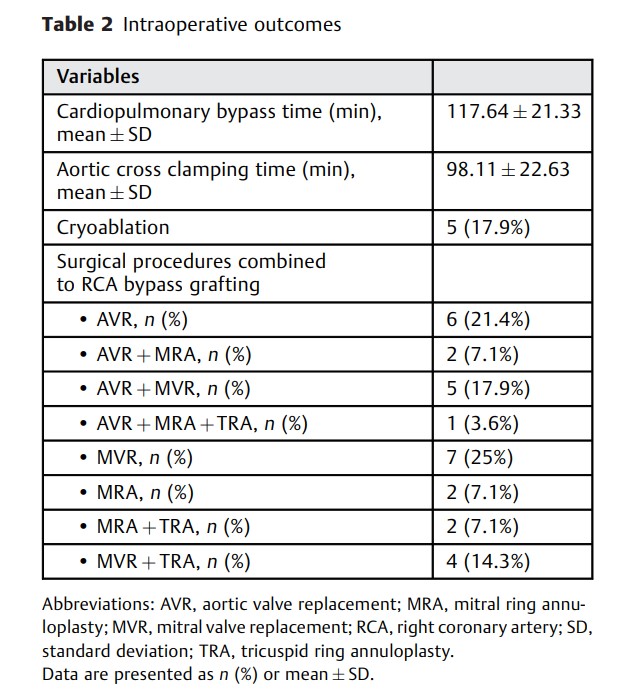
Hasde et al.
Patients with combined valve and coronary artery disease are commonly performed by standard median sternotomy approach for coronary artery bypass grafting (CABG) and valve surgery. The purpose of this study is to describe our experience and show feasibility and safety of minimally invasive approach to single or combined valve pathology with single-vessel right coronary artery (RCA) disease, even if it is suitable to percutaneous coronary intervention.
AORTA
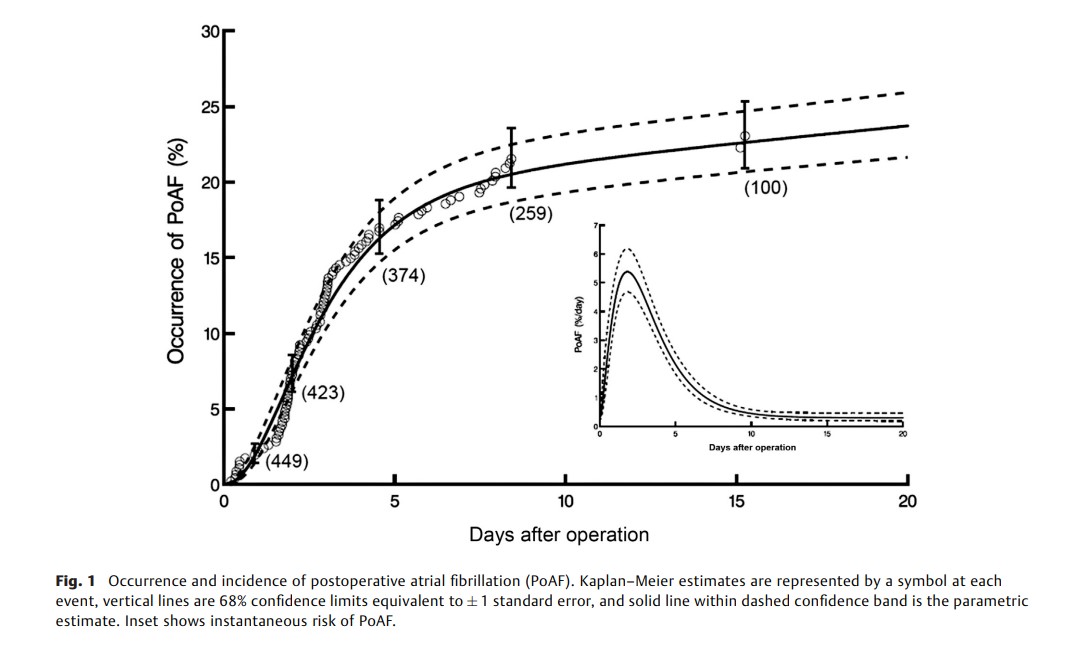
Atrial Fibrillation after Descending Aorta Repair: Occurrence, Risk Factors, and Impact on Outcomes
Pujara et al.
As risks of repairing the descending thoracic and thoracoabdominal aorta diminish, common complications that may prolong hospital stay, or actually increase risk, require attention. One such complication is postoperative atrial fibrillation (AF). Therefore, we characterized prevalence of, risk factors for, and effects of postoperative atrial fibrillation (PoAF) after descending and thoracoabdominal aorta repair.
The Thoracic and Cardiovascular Surgeon Report
Coronary Anastomosis In Stent—Useful to Do When No Other Alternative Is Given?
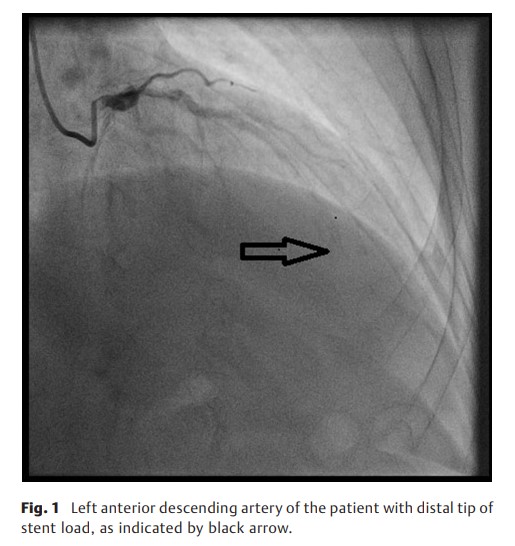
Balan et al.
In a patient after multiple PCI of the left anterior descending artery (LAD), repeated in-stent stenosis was diagnosed. The LAD being covered with stents to the periphery, no meaningful anastomosis with stent-free vessel was possible. After thorough discussion with the patient, the referring cardiologist, and our local heart team, an in-stent anastomosis was planned and created, that was found to be angiographically patent 21 months after surgery with the patient free from angina.